Washington Post Won’t Say Why Trust in Vaccines Is Gone
Until public health authorities—and the media that defend them—are willing to acknowledge Covid-era failures openly, trust will not be restored.
BY ROGER BATE
View original article at Brownstone.org.
The Washington Post recently published a detailed investigation showing that childhood vaccination rates across the United States are falling sharply, particularly for measles. Fewer counties now meet the 95 percent coverage level commonly associated with herd immunity, and millions of children attend schools in communities below that threshold.
On the basics, it’s true that routine childhood measles shots are among the most effective measures for keeping that particular infection at bay. But the Post’s analysis fails where it matters most: it cannot explain why trust has collapsed so broadly, so persistently, and so rationally for many ordinary people.
Instead, readers are offered a familiar diagnosis. Distrust of authorities. Political polarization. Misinformation. Backlash against mandates. All of this is curiously detached from responsibility. The article describes the consequences of distrust without confronting its causes.
That omission is not accidental. It reflects a broader unwillingness among elite media and public health institutions to reckon honestly with Covid-era failures. And without that reckoning, efforts to restore vaccine confidence are unlikely to succeed.
This is not an argument against vaccines. It is an argument about credibility.
During the Covid-19 period, public health authorities repeatedly overstated certainty, minimized uncertainty, and treated legitimate scientific disagreement as a threat rather than a feature of good science.
Claims about vaccines preventing infection and transmission were presented as settled fact, not evolving hypotheses. When those claims weakened or collapsed under new evidence, they were revised quietly, without acknowledgment of error.
The same pattern appeared across other policies: masking, school closures, natural immunity, and population-level risk. Positions shifted, sometimes dramatically, but rarely with public explanation. The message conveyed—intentionally or not—was that narrative management mattered more than transparency.
This mattered because trust is cumulative. People do not evaluate each public health recommendation in isolation. They judge institutions based on patterns of behavior over time. When authorities insist they were always right, even when claims visibly change, credibility erodes.
Worse, dissent was often suppressed rather than debated. Scientists and clinicians who questioned prevailing policies—on lockdowns, school closures, or mandates—were frequently labeled as misinformation spreaders rather than engaged on the merits. Government coordination with social media platforms blurred the line between combating falsehoods and policing debate. Once that line is crossed, institutional trust does not merely decline—it inverts.
None of this requires assuming bad faith. Emergencies are hard. Decisions were made under pressure. But good faith does not excuse overstatement, nor does difficulty justify refusing retrospective evaluation.
The result of this approach is now visible in the data the Washington Post reports—but does not explain.
Evidence from Pennsylvania illustrates the point. Montgomery County, a large, affluent, highly educated Philadelphia suburb, has historically had strong vaccination uptake and robust healthcare access. It is not a place easily dismissed as anti-science or anti-medicine.
Yet my physician survey research conducted in the county during and after the pandemic tells a different story. Clinicians reported that while initial Covid vaccine uptake was high in 2021, acceptance declined sharply over time, particularly for boosters. More importantly, many physicians observed a spillover effect: growing hesitancy not only toward Covid vaccines, but toward other vaccines as well.
Patients were not primarily citing technical fears about vaccine safety. They were expressing distrust of public health authorities. They referenced shifting claims, perceived exaggeration, and the absence of acknowledgment of error. Named figures—most notably Dr. Anthony Fauci—were mentioned not as sources of reassurance, but as symbols of lost credibility.
Ongoing follow-up work in Montgomery County suggests this dynamic is not fading. Hesitancy appears to be hardening, increasingly framed not as uncertainty about specific vaccines, but as refusal to rely on institutions that have never conducted a transparent review of their pandemic performance. The absence of any meaningful Covid audit is frequently cited as a reason for continued distrust.
The Washington Post notes “distrust of authorities” but treats it as a sociological condition rather than a consequence of institutional behavior. That framing is convenient, but it is incomplete. Distrust did not emerge from nowhere. It was earned.
This matters for policy because different causes demand different solutions. If vaccine hesitancy were primarily driven by ignorance about vaccine science, then more education and clearer messaging might suffice. But when hesitancy is rooted in governance failure—overconfidence, suppression of debate, refusal to acknowledge mistakes—messaging alone will not work. In fact, it may backfire.
What is missing is accountability—not punishment, not jail, not tribunals—but acknowledgment.
In every other domain of public life, major failures are followed by audits. Financial crises, industrial accidents, intelligence breakdowns, transportation disasters—all prompt formal reviews aimed at understanding what went wrong and how to do better. These processes are not about retribution. They are about restoring confidence that institutions can learn.
Covid has been the exception.
There has been no comprehensive, independent, and transparent review of pandemic decision-making in the United States. Agencies have issued self-assessments, but these emphasize difficulty rather than error. Senior officials rarely concede specific mistakes. Media coverage largely treats criticism as politically motivated rather than analytically serious.
The result is a lingering credibility deficit. Each new public health recommendation—whether about boosters, childhood vaccines, or unrelated interventions—is filtered through the unresolved memory of Covid. People are not asking whether measles vaccines worked in 1965. They are asking whether they can trust institutions that refuse to reflect honestly on 2020–2022.
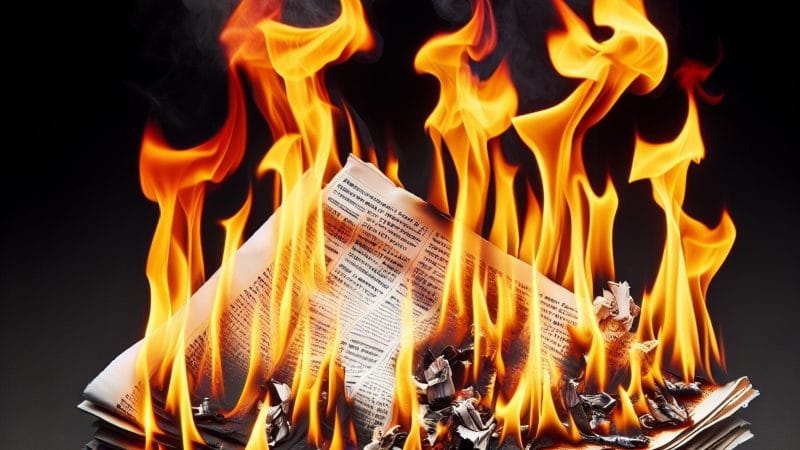
The Washington Post is right to warn about falling vaccination rates. But by refusing to confront the institutional roots of distrust, it is not part of the solution. It documents the smoke while declining to examine the fire.
Measles immunity matters. But so should elite misinformation, overstatement, and institutional defensiveness.
Until public health authorities—and the media that defend them—are willing to acknowledge Covid-era failures openly, trust will not be restored. And without trust, even the best vaccines will struggle to achieve the coverage they deserve.
The problem is not that science failed. It is that institutions have not yet admitted where they did.


The article very casually says: "On the basics, it’s true that routine childhood measles shots are among the most effective measures for keeping that particular infection at bay. "
The statement seems to assume that this is a well known fact. But how do we know that? No proper testing has been done for any vaccine.
Many people say that the American people have very short memory span, but especially so for people who have publicly repented their sins and conceded that they made mistakes. Of course, people would watch this guy more closely after the event, but few would try to browbeat the sinner repeatedly using events of the past.
Unfortunately, that kind of honesty for being willing to concede errors seems to have long gone in the US. Maybe that is why the elementary school textbooks keep on touting the story of Washington felling his father's cherry trees, because modern people simply don't do that anymore.
But once we start talking about the "elites" in societies, then they seem to lie through their teeth routinely, because they think they cannot afford to confess failures or mistakes. Then you have the kind people who think they are God himself. These people will never confess a failure or mistake in public. They will hire an assassin to solve "the problem" before they do that.
I think it is less of an issue about "more willing to lie", but rather an issue of "cannot confess/concede failures or errors". If lying happens to be the most handy tool to "handle the situation", then they will lie. Or they could choose to do something else. Such as Pfizer trying to buy out some professors making important diagnostics about spike proteins from vaccines causing cancers. Or even the execution of the UHC chief (I don't think it was a robinhood-like operation, but rather more like a potential corporate policy change will block somebody's money spigot or reveal somebody else's mistakes.)